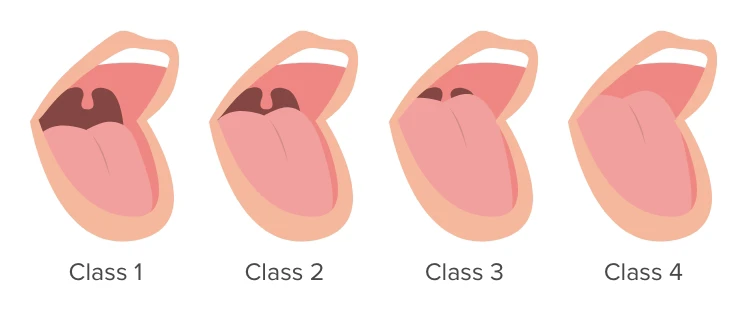
If a doctor asks you to open wide, stick out your tongue, and say "ah," they might be doing more than checking for a sore throat. The Mallampati classification — a quick look at how much of your throat structures (uvula, soft palate, tonsillar pillars) are visible — was created to predict how difficult it might be to place a breathing tube during anesthesia. Over time, clinicians noticed that a crowded-looking throat (a high Mallampati class) also seems to show up more often in people with obstructive sleep apnea (OSA).1
So what is Mallampati, in plain English?
It's a 1–4 scale based on what an examiner can see when you open your mouth and stick out your tongue: Class I = easy view of throat structures; Class IV = only the hard palate visible. Higher classes mean a smaller space in the back of the throat, which could make the airway more likely to collapse during sleep — the hallmark of OSA. 1
Can Mallampati help predict OSA risk?
Short answer: sometimes. Multiple studies and reviews have shown that higher Mallampati scores are more common in people with moderate-to-severe OSA, and adding Mallampati to other simple measures (like neck size, age, BMI, or snoring questionnaires) can improve prediction models. For example, one study found that combining Mallampati >2 with age and neck circumference gave a high probability of moderate-to-severe OSA in patients already suspected of sleep apnea.2,3,7
But, and this is important, Mallampati is not a perfect screen. Some research cautions that Mallampati alone doesn't reliably rule OSA in or out when used by itself in general clinic populations. Other systematic reviews and sleep-physical-exam studies recommend using Mallampati as one piece of the puzzle, not the whole picture. Examiner technique, patient posture, whether the patient phonates, and natural anatomical variation all affect the score.4,5,6
What does that mean for you?
If your Mallampati class is high, it may raise suspicion for OSA — especially when combined with symptoms (daytime sleepiness, loud snoring, witnessed apneas) or other risk factors. Conversely, a low Mallampati score doesn't guarantee you're free of sleep apnea. Most sleep specialists use questionnaires, physical exam findings (including Mallampati), and — when indicated — a sleep test (home or lab) to make a diagnosis.5,7
The bottom line:
The Mallampati classification is a quick, noninvasive clue about throat anatomy and can add value in assessing OSA risk, especially as part of combined screening tools. However, it's not sufficiently reliable to be used alone as a definitive screen or a substitute for formal sleep evaluation when OSA is suspected. If you're worried about sleep apnea, mention your sleep symptoms and any exam findings to a clinician — the Mallampati score may help nudge the decision toward further testing, but it's rarely the last word. 1,5
References:
- NCBI Mallampati Score
- PubMed The prediction of obstructive sleep apnea severity based on anthropometric and Mallampati indices
- PubMed Tongue size matters: revisiting the Mallampati classification system in patients with obstructive sleep apnea
- Mallampati Class Is Not Useful in the Clinical Assessment of Sleep Clinic Patients
- PMC The Obstructive Sleep Apnea Physical Exam: A Systematic Review and Meta‐Analysis
- Sleep Foundation. Mallampati Score and Predicting Sleep Apnea
- Journal of Clinical Sleep Medicine. Utility of the modified Mallampati grade and Friedman tongue position in the assessment of obstructive sleep apnea